If your child is struggling, you’re not alone — and neither are they. Mental health challenges are common in childhood and adolescence, and the way we respond can shape a child’s wellbeing into adulthood. This guide focuses on what parents can do today: how to find professional help, what the research suggests, and simple, science-backed strategies you can start at home.
Important: This article is educational and not medical advice. If you’re worried about immediate safety, contact local emergency services or a crisis hotline right away.
Getting Professional Help (Start Here)
When a child is struggling, a licensed professional can help you create a tailored plan. Pediatricians, child psychologists, and school counselors can coordinate care and point you to local resources. Many families also review general guidance like internet safety tips for parents to reduce online stressors while they’re waiting for appointments.
Finding care: National directories (e.g., psychology associations), hospital clinics, school-based counseling, and community nonprofits can shorten the search. If waitlists are long, ask about group programs or telehealth options.
In a crisis: Use your local emergency number or a national crisis line in your country. Keep those numbers saved and visible.
Parent Perspective: Why You Matter So Much
Strong, steady relationships with caring adults are among the most protective factors in child development. That means how you connect daily — listening, co-regulating, setting warm boundaries — really moves the needle.
Conversations about tough topics often go better when you practice ahead using prompts from how to talk to your child about inappropriate pictures or follow-ups from what to do if your child sends inappropriate pictures.
Strategy 1: Build Social-Emotional Skills (SEL) at Home
What it is: Social-emotional learning teaches kids to name feelings, manage stress, solve problems, and nurture relationships. These skills buffer anxiety and depression and improve school outcomes.
At-home ideas (10–15 min/day):
Do a quick “feelings check-in,” then pick a coping tool (breathing, movement, drawing). You’ll find age-friendly ideas in mental health activities for kids.
Practice small acts of kindness; prosocial behavior often lifts mood.
Use creative outlets — music, drawing, storytelling — to process emotions.
When screens escalate emotions, families often revisit why parents should limit screen time and choose calmer replacements from their coping menu.
Strategy 2: Create a Supportive Daily Environment
Routines reduce anxiety. A predictable flow for mornings, homework, movement, meals, and bedtime helps kids feel safe and in control.
Make it practical:
Post a simple visual schedule and review it together each morning.
Design a calm corner with a few sensory items and a feelings chart.
Set clear, kind boundaries and explain the “why.” Expect pushback; follow through calmly.
For schoolwork or online time, minimize triggers by applying what you use elsewhere, e.g., rules you learned from how to prevent cyberbullying or device norms you set during a detox child from screen time.
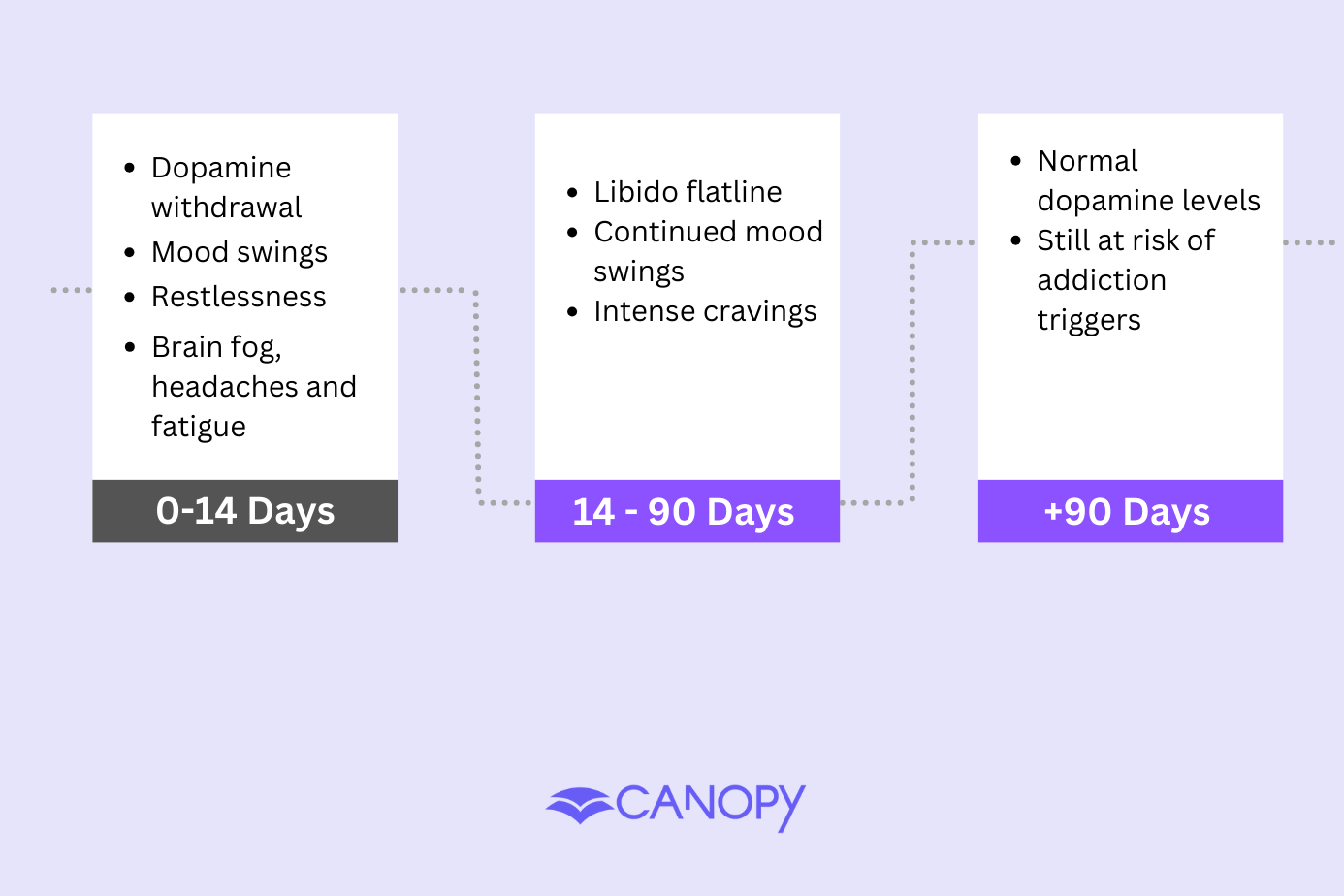
Strategy 3: Understand Today’s Digital Stressors
Many kids face persistent online pressures: cyberbullying, comparison spirals, sexual solicitation, and exposure to explicit content. You can lower risk by tightening privacy, curating feeds, and using tools thoughtfully.
When social apps spike anxiety, review family rules and reinforce media breaks.
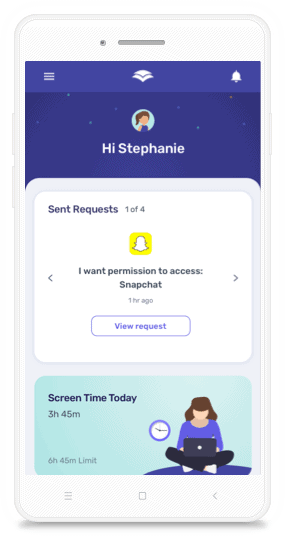
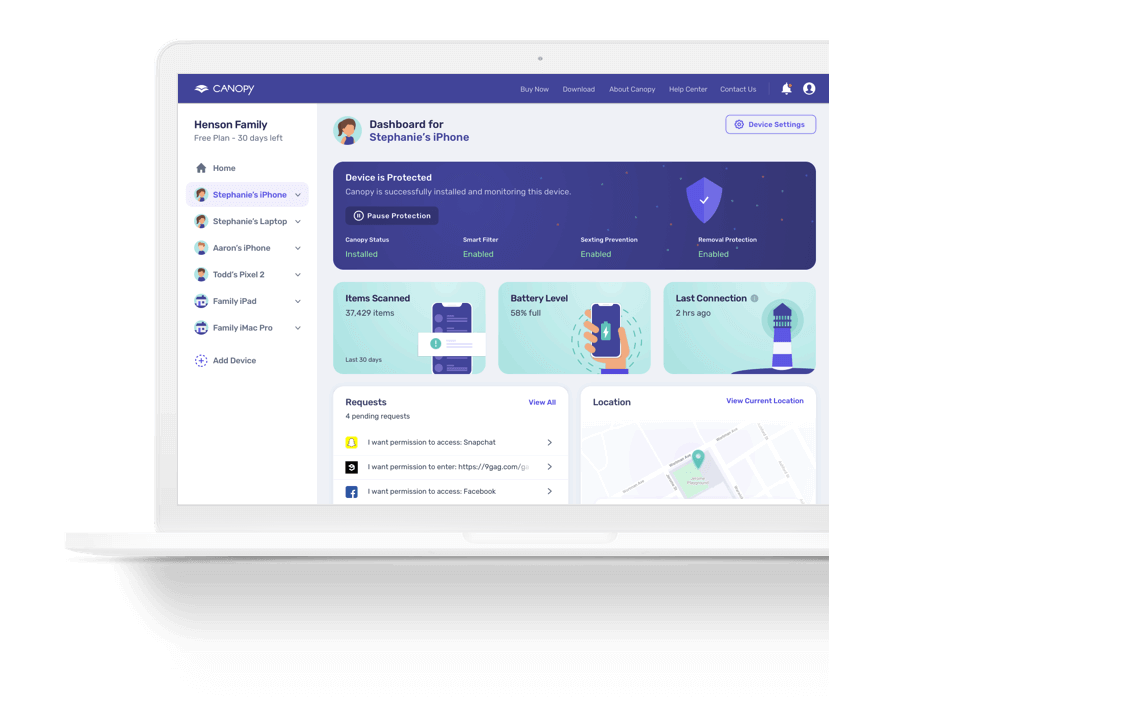
If you need tech help beyond device settings, some families use a parental control app to shape access, or a text monitoring app to surface red flags while conversations continue.
If your child uses short-form video, adapt steps from TikTok parental controls to reduce harmful recommendations.
Strategy 4: Normalize Treatment—and Start Early
Stigma keeps many families from getting care. Treat mental health support like any other health need.
Seek help early. Even brief interventions can prevent symptoms from worsening.
Stick with providers when you find a good fit; continuity builds trust.
Track patterns (sleep, mood, triggers) in a simple diary to share at appointments.
Note family history to inform screening and prevention.
Strategy 5: Care for Yourself (It’s Part of the Plan)
Your well-being is a core intervention. Caregivers under chronic stress have less bandwidth for co-regulation.
Schedule rest, movement, and meals as non-negotiables.
Join a parent support group to learn skills and feel less alone.
Share the load—ask relatives or friends for concrete help so you can recharge.
Add small “joy anchors” to the week (walk with a friend, art night, music).
FAQs
How do I explain “mental health” to a child?
Use simple analogies (“Our brains can get sick like our stomachs do”) and name body cues (tight chest, wobbly tummy). Short stories can make it concrete.
What are warning signs to watch for?
Persistent sadness, major sleep/appetite changes, withdrawal, intense worry, self-harm talk or behaviors, aggression, substance use, or big personality shifts. If anything feels unsafe, seek urgent help.
What helps kids with depression day to day?
Gentle routine, enjoyable movement, steady sleep, nourishing food, and low-pressure social contact. Creative outlets can help externalize feelings
What supports a child with anxiety?
Name feelings, practice grounding (5-4-3-2-1 senses), and teach slow breathing. Keep bedtimes consistent, and reduce digital overload.